1.Carvalho P. et al, Clinical Research in Cardiology, Received: 22 September 2022 / Accepted: 21 December 2022 , Published online 2 Jan 2023, https://doi.org/10.1007/s00392-022-02148-2
2. Braunwald E., SGLT2 inhibitors: the statins of the 21st century, European Heart Journal (2022) 43, 1029–1030, https://doi.org/10.1093/eurheartj/ehab765
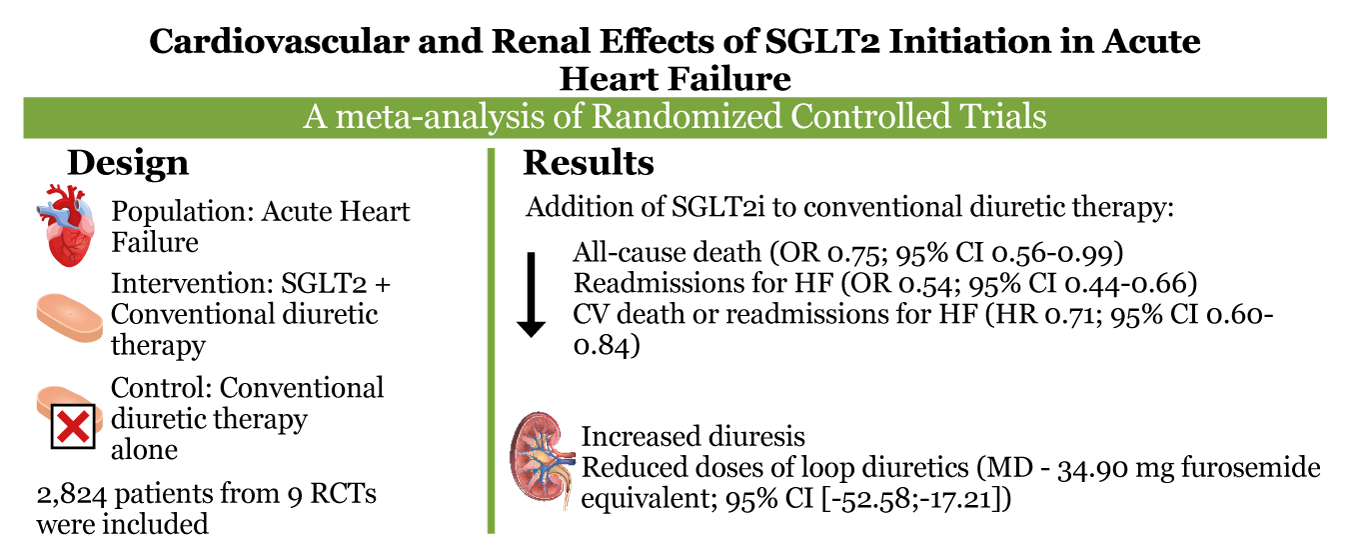
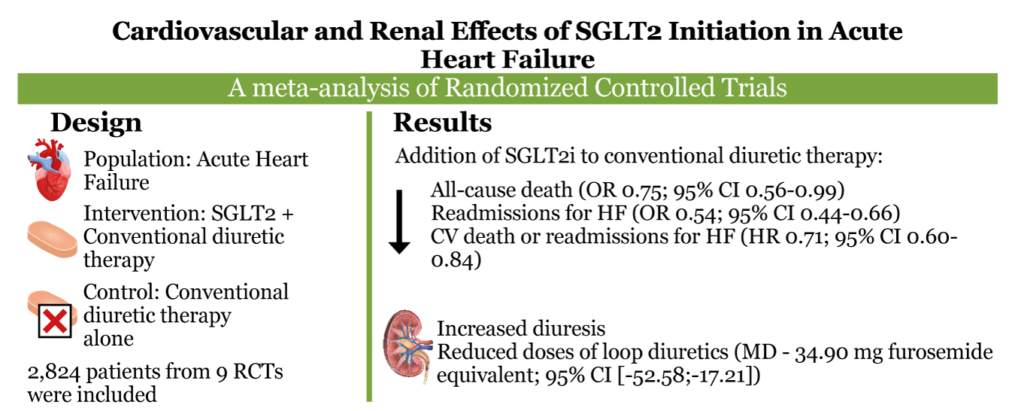
Background We sought to compare cardiovascular outcomes, renal function, and diuresis in patients receiving standard diuretic therapy for acute heart failure (AHF) with or without the addition of SGLT2i.
Acute heart failure (AHF) is the leading cause of unplanned hospitalization in those over 65 years and is characterized by new-onset or worsening symptoms of heart failure (HF). Most patients with AHF are admitted with evidence of fluid overload and are generally treated with escalating doses of intravenous loop diuretics to improve symptoms and reduce morbidity. However, this diuretic regimen is limited by worsening renal function and many patients do not obtain adequate decongestion during the hospital stay for AHF. In fact, current treatment for AHF has not changed significantly in decades. Unsurprisingly, post discharge outcomes have remained poor with 30-day readmission and 1-year mortality rates being as high as 20–30%. Therefore, there is an unmet need for new therapeutic strategies in this population.
In recent years, sodium-glucose cotransporter 2 inhibitors (SGLT2i) have been proved to be effective in the treatment of HF for reducing cardiovascular mortality and hospitalizations, regardless of diabetes or ejection fraction status. SGLT2i also reduce the composite outcome of cardiovascular death or deterioration of renal function in patients with chronic kidney disease (CKD). However, less is known about the safety and efficacy of adding SGLT2i to conventional diuretic therapy in patients admitted with AHF.
A prior meta-analysis examining this issue found a reduction in rehospitalizations for HF in patients treated with SGLT2i. However, there was no significant decrease in mortality with SGLT2i, which may have been related to limited power . Therefore, we aimed to perform an updated systematic review and meta-analysis of randomized controlled trials (RCTs) comparing conventional diuretic therapy with or without concomitant SGLT2i for cardiovascular and renal endpoints in patients with AHF.
Methods and results
Systematic search of three electronic databases identified nine eligible randomized controlled trials involving 2,824 patients. The addition of SGLT2i to conventional therapy for AHF reduced all-cause death (odds ratio [OR] 0.75; 95% CI 0.56–0.99; p = 0.049), readmissions for heart failure (HF) (OR 0.54; 95% CI 0.44–0.66; p < 0.001), and the composite of cardiovascular death and readmissions for HF (hazard ratio 0.71; 95% CI 0.60–0.84; p < 0.001). Furthermore, SGLT2i increased mean daily urinary output in liters (mean difference [MD] 0.45; 95% CI 0.03–0.87; p = 0.035) and decreased mean daily doses of loop diuretics in mg of furosemide equivalent (MD -34.90; 95% CI [− 52.58, − 17.21]; p < 0.001) without increasing the incidence worsening renal function (OR 0.75; 95% CI 0.43–1.29; p = 0.290).
Conclusion
SGLT2i addition to conventional diuretic therapy reduced all-cause death, readmissions for HF, and the composite of cardiovascular death or readmissions for HF. Moreover, SGLT2i was associated with a higher volume of diuresis with a lower dose of loop diuretics.
Some Facts about SGLT2i 2
- Between 2012 and 2015, the European Medicine Agency (EMA) and the US Food and Drug Administration (FDA) approved three SGLT2is, dapagliflozin, canagliflozin, and empagliflozin, for reducing plasma glucose in persons with T2DM
- SGLT2i are not only glucosuric but also reduce the development and progression of heart failure and prolong life in patients with T2DM and reduced left ventricular ejection fraction
- SGLT2i improve outcomes in patients with HFrEF irrespective of the presence or absence of T2DM, thereby greatly expanding the potential target population for these drugs.
- SGLT2i appear to be beneficial in patients with chronic heart failure over a wide range of ejection fractions, again greatly expanding the target population even further.
- SGLT2i slow the development of end-stage kidney disease in patients with chronic kidney disease. The benefit of SGLT2i in patients without T2DM but with a variety of chronic kidney diseases is under investigation.