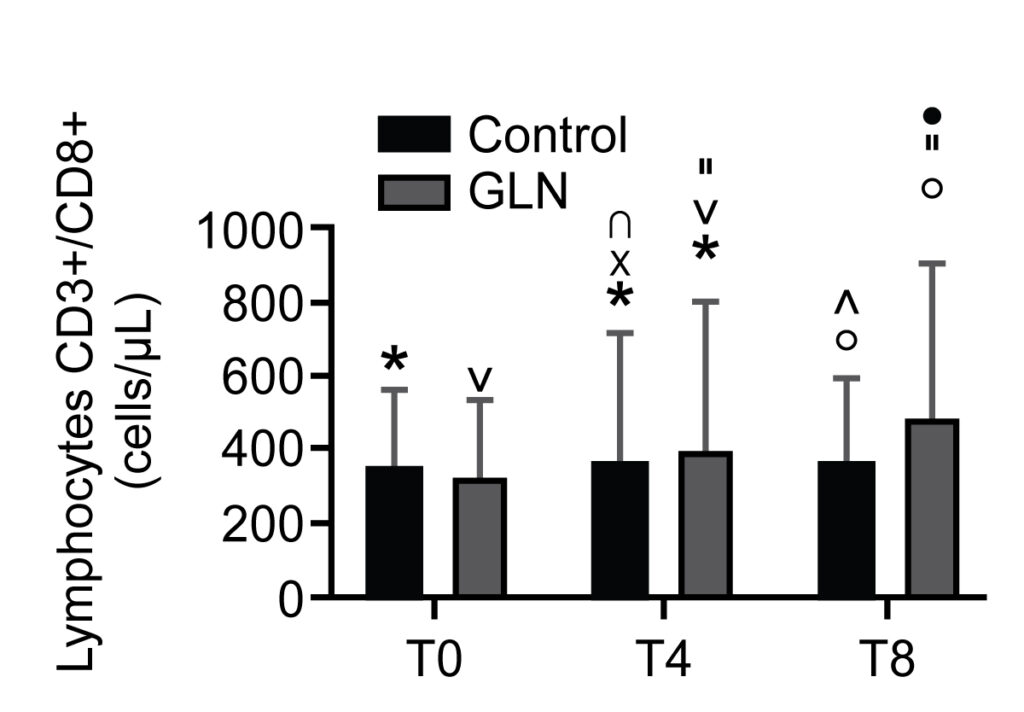
Ref: Cotoia et al. J Anesth Analg Crit Care (2022) 2:41, https://doi.org/10.1186/s44158-022-00068-1
Glutamine (GLN) is classified as a non-essential amino acid and it is released from skeletal muscle to be a constituent of proteins . Furthermore, GLN acts as an immune stimulator as an essential component for lymphocyte proliferation and cytokine production, macrophage phagocytic and secretory activities, and neutrophil bacterial killing . Under stable conditions, GLN can be produced in suffcient amounts and stored in the muscle tissue. Tese stores actually represent greater than 50% of the total free amino acid pool in the body.
However, GLN levels normally decrease in intensive care unit (ICU) patients both due to a hypercatabolic status, especially in trauma and sepsis, and an increased requirement by the gut, the immune system, liver and kidneys which exceeds the individual’s ability to produce it in sufficient amounts. In critically ill patients, GLN may even become a “conditionally essential” amino acid : it is considered a “fuel for the immune system”, where a low blood concentration may impair immune cell function, resulting in poor clinical outcomes and increased risk of mortality, and so its supplementation is recommended in ICU patients . Interestingly, some authors showed that GLN supplements of 10–20 g/day (or with a high dose >0.2g/kg/day) plus standard enteral nutrition (EN) formulas reduced the rates of pneumonia, sepsis and bacteraemia in ICU patients with shortened hospital stays, better immune function and lower hospital costs .
It is important to note that humoral immunity is a process of adaptive immunity mediated by immunoglobulins such as IgA secreted by B lymphocytes . Cell-mediated immunity is responsible for destroying the intracellular pathogens with T lymphocytes, which consequently produce inflammatory mediators such as interleukin. More clinical trial and new studies on these topics are necessary to focus on cell-mediated and humoral immune responses in severely injured trauma patients and rule on GLN depletion on immune functioning . We hypothesize that GLN could enhance both humoral and cell-mediated immunity. The aim of our study is to investigate the effect of GLN-enriched EN on the cell mediated and humoral immune system in ICU polytrauma patients.
Methods:
All consecutive patients with polytrauma who required mechanical ventilation and enteral nutrition (EN) provided within 24 h since the admission in ICU at the University Hospital of Foggia from September 2016 to February 2017 were included.
Thereafter, two groups were identifed: patients treated by conventional EN (25 kcal/kg/die) and patients who have received conventional EN enriched with 50 mg/kg/ideal body weight of alanyl-GLN 20% intravenously.
We analysed the plasmatic concentration of IgA, CD3+/CD4+ T helper lymphocytes, CD3+/CD8+ T suppressor lymphocytes, CD3+/CD19+ B lymphocytes, IL-4 and IL-2 at admission and at 4 and 8 days.
Results:
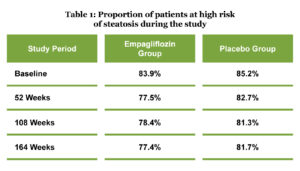
IgA levels in control and glutamine (GLN) groups. Data are presented as mean ± SD. °, * and ^ indicate a significant difference in GLN vs control at T0 (p < 0.05), at T4 (p < 0.05), and at T8 (p < 0.01); • indicates a significant difference (p < 0.05) in the GLN group between T4 and T8
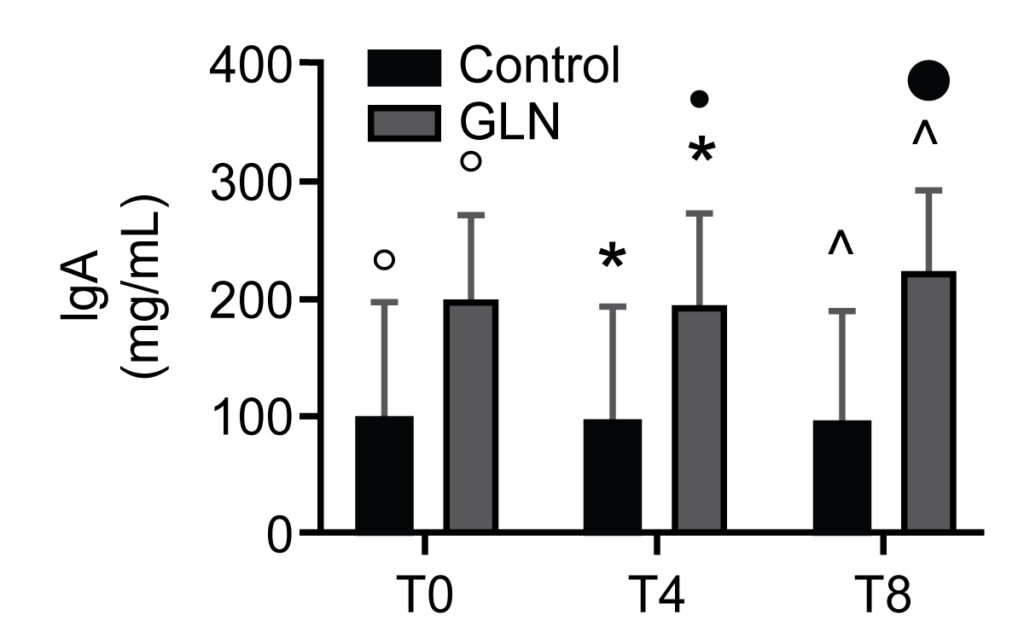
CD3+/CD4+ T helper lymphocyte levels in control and glutamine (GLN) groups. Data are presented as mean ± SD. *, °, and ^ indicate a significant difference in GLN vs control at T4 (p < 0.01) and T8 (p < 0.001); ˅, ”, and • indicate statistically highly significant (p < 0.001) in the GLN group
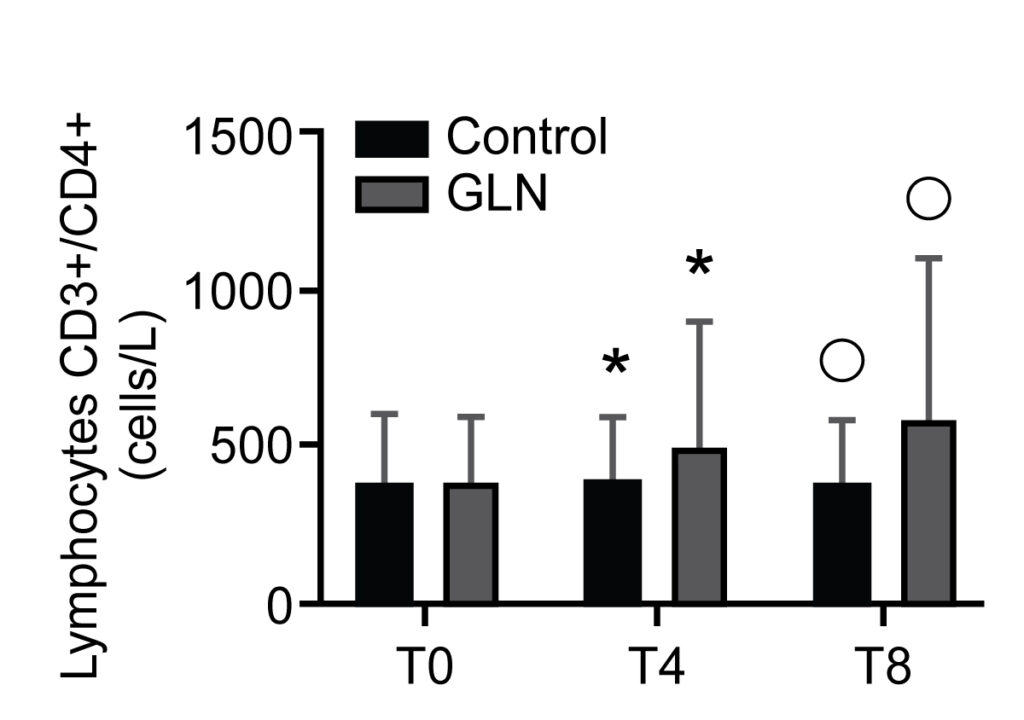
CD3+/CD8+ T suppressor lymphocyte levels in control and glutamine (GLN) groups. Data are presented as mean ± SD. * and °indicate a significant difference in GLN vs control at T4 (p < 0.05) and at T8 (p < 0.001); ˅, ”, and • indicate statistically significant (p < 0.001) in the GLN group; x and ∩ indicate a significant difference in the control group between T0 and T4 (p < 0.001) and T4 and T8 (p = 0.002)
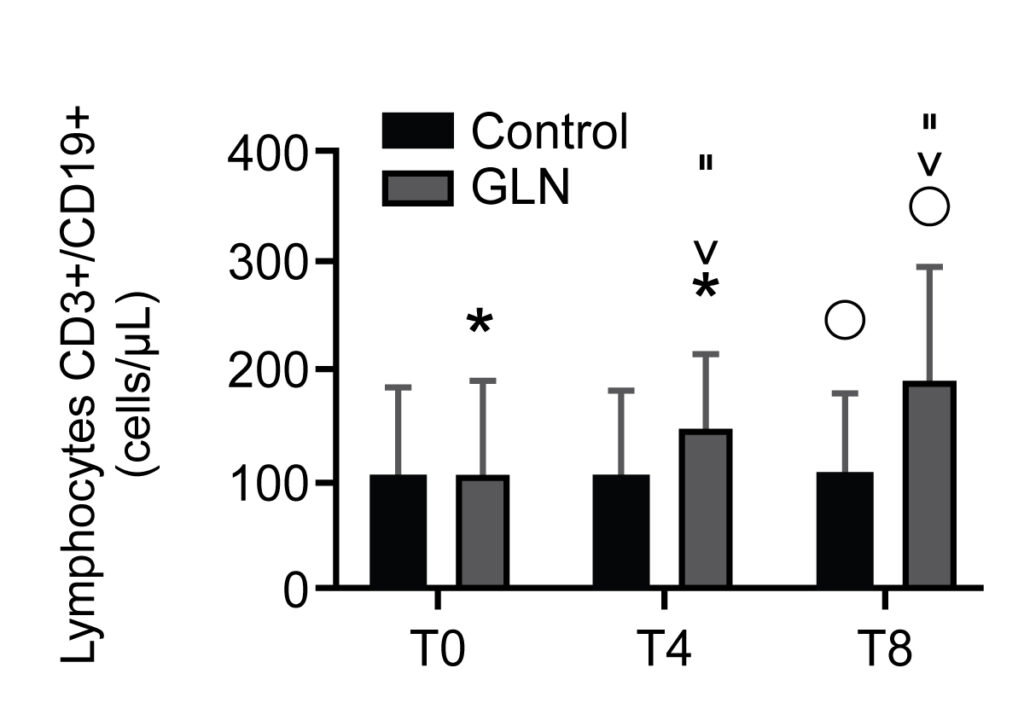
B lymphocyte CD3+/CD19+ levels in control and glutamine (GLN) groups. Data are presented as mean ± SD. “indicate a significant difference in GLN vs control at T8 (p = 0.01); *, ˅, and ” indicate statistically highly significant (p < 0.001) in the GLN group
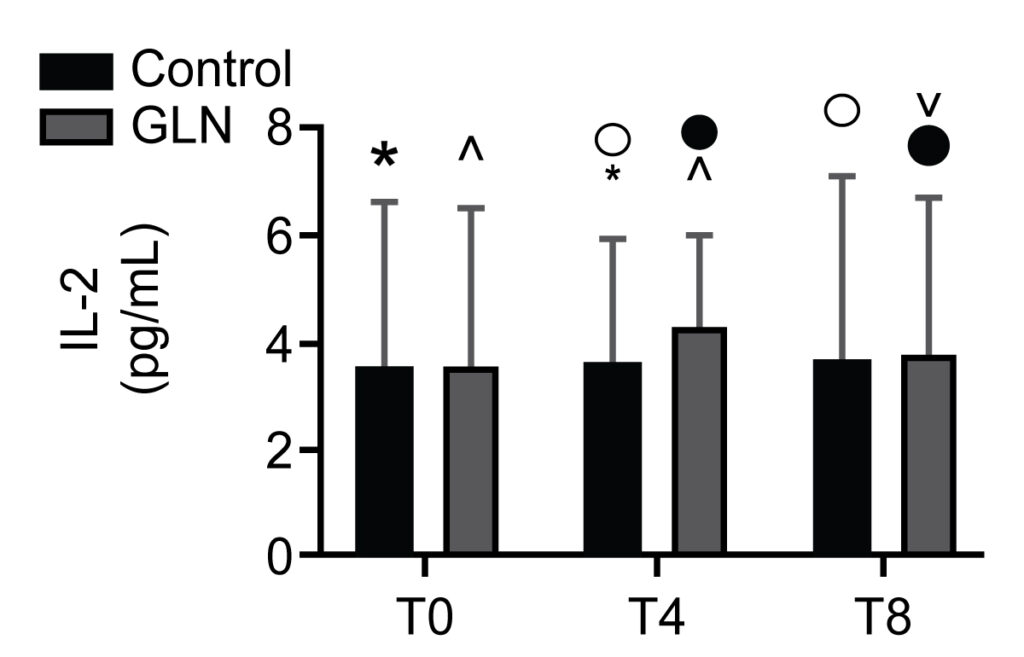
IL-2 levels in control and glutamine (GLN) groups. Data are presented as mean ± SD. ^, •, and ˅ indicate a significant difference in the GLN group (p < 0.05); * and ° indicate a significant difference in the control group between T0 and T4 (p = 0.002) and T4 and T8 (p = 0.002)
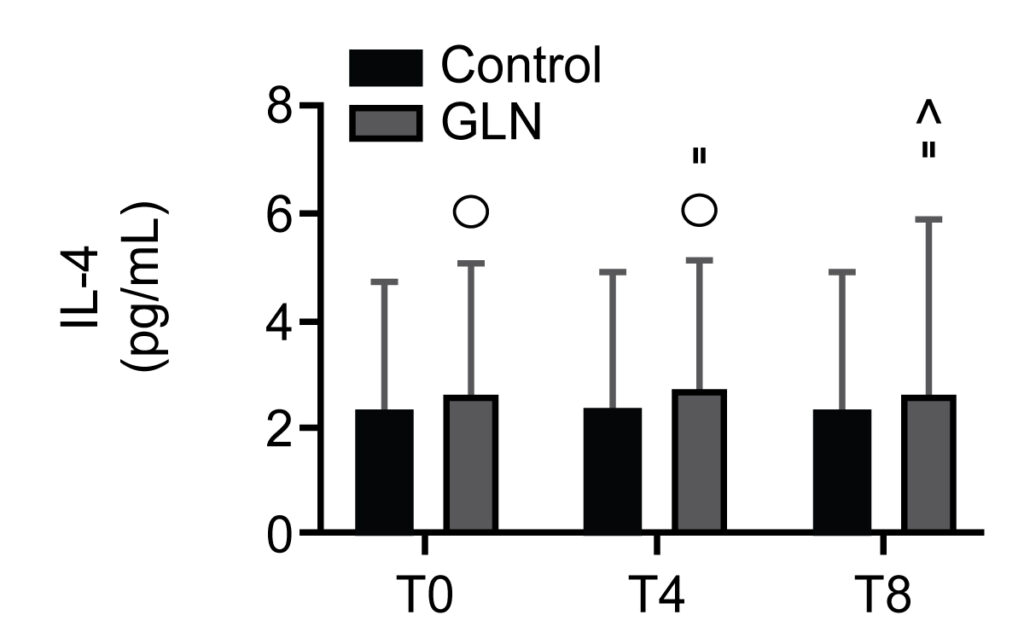
IL-4 levels in control and glutamine (GLN) groups. Data are presented as mean ± SD. °, ”, and ^ indicate a significant difference (p < 0.004) in the GLN group
Results:
We identified 30 patients, with 15 subjects per group. IgA levels increased significantly in GLN vs the control group at T0, T4 and T8. CD3+/CD4+ T helper lymphocyte and CD3+/CD8+ T suppressor lymphocyte levels significantly increased in GLN vs the control group at T4 and T8. CD3+/CD19+ B lymphocyte levels increased significantly in GLN vs the control group only at T8. IL-2 and IL-4 levels showed no significant differences when comparing GLN with the control group.
Conclusions:
Our study showed that there was an improvement in humoral and cell-mediated immunity with GLN supplementation in polytrauma ICU patients using recommended doses.