Conservative rates of dextrose infusion can mitigate the risk for hyperglycemia in hospitalized adults with obesity who are receiving parenteral nutrition (PN), as shown in findings presented at the ASPEN 2022 Nutrition Science and Practice Conference. Moreover, obesity alone does not predict the likelihood of hyperglycemia during PN administration.
“Hyperglycemia is a well-described metabolic complication of parenteral nutrition in any patient, but obese adult hospitalized patients may be at an elevated risk, given the higher prevalence of insulin resistance and glucose intolerance in these individuals,” said Angela Bingham, PharmD, the vice chair and an associate professor of clinical pharmacy at Philadelphia College of Pharmacy.
To determine the effect of obesity on glycemic control in adult hospitalized patients started on PN, Dr. Bingham and her colleagues retrospectively studied 646 adult patients hospitalized from 2013 to 2021, who received at least two consecutive days of PN. The group included 205 obese patients with a body mass index (BMI) of at least 30 kg/m2; the median BMI for obese and nonobese patients was 35.55 and 23.85 kg/m2, respectively. The researchers defined a hyperglycemic episode as a blood glucose level above 200 mg/dL.
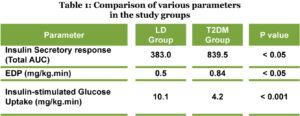
According to Dr. Bingham, obese patients were younger than nonobese patients (median age, 58 vs. 62 years), more likely to have critical illness (42% vs. 29.7%) and diabetes mellitus (35.6% vs. 18.1%), and had higher serum creatinine levels (median, 0.84 vs. 0.76 mg/dL) (P<0.05 for all). Nearly all patients received PN through a central line.
Dextrose infusion rates for obese patients were lower than for nonobese patients, at 1.66 and 1.92 mg/kg per minute, on day 1 of PN (P<0.0001) and 2.62 and 2.79 mg/kg per minute on day 2 (P=0.0003).
Dr. Bingham told meeting attendees that hyperglycemic episodes were infrequent in both groups on days 1 and 2 of PN, but occurred significantly more commonly in obese patients (0.89 vs. 0.52; P<0.05).
However, multivariate analyses that adjusted for potential confounders, including age, critical illness, Charlson Comorbidity Index score, cerebrovascular disease, diabetes mellitus, serum creatinine, creatinine clearance, serum osmolarity, baseline hyperglycemia and macronutrient provision found that obesity was not an independent predictor of hyperglycemic episodes (odds ratio [OR] on day 1, 1.047; 95% CI, 0.639-1.717; P=0.8551 and OR on day 2, 0.964; 95% CI, 0.611-1.521; P=0.8758).
“Our experience shows that conservative dextrose infusion rates may minimize the risk of hyperglycemia in adult hospitalized patients with obesity receiving parenteral nutrition, and that obesity is not an independent predictor of hyperglycemic episodes during the first two days of parenteral nutrition initiation,” Dr. Bingham said. She added that her institution’s guidelines of “vigilant” blood glucose concentration monitoring every four to six hours in PN recipients may have also contributed to the low rates of hyperglycemia.