Ref: Le Pape et al. Annals of Intensive Care (2022) 12:24, https://doi.org/10.1186/s13613-022-00998-7
Background
The clinical impact and outcomes of ventilator-associated pneumonia (VAP) have been scarcely investigated in patients with the acute respiratory distress syndrome (ARDS).
Methods
Patients admitted over an 18-month period in two intensive care units (ICU) of a university-affiliated hospital and meeting the Berlin criteria for ARDS were retrospectively included. The association between VAP and the probability of death at day 90 (primary endpoint) was appraised through a Cox proportional hazards model handling VAP as a delay entry variable. Secondary endpoints included (i) potential changes in the PaO2/FiO2 ratio and SOFA score values around VAP (linear mixed modelling), and (ii) mechanical ventilation (MV) duration, numbers of ventilator- and vasopressor-free days at day 28, and length of stay (LOS) in patients with and without VAP (median or absolute risk difference calculation). Subgroup analyses were performed in patients with COVID-19-related ARDS and those with ARDS from other causes.
Results
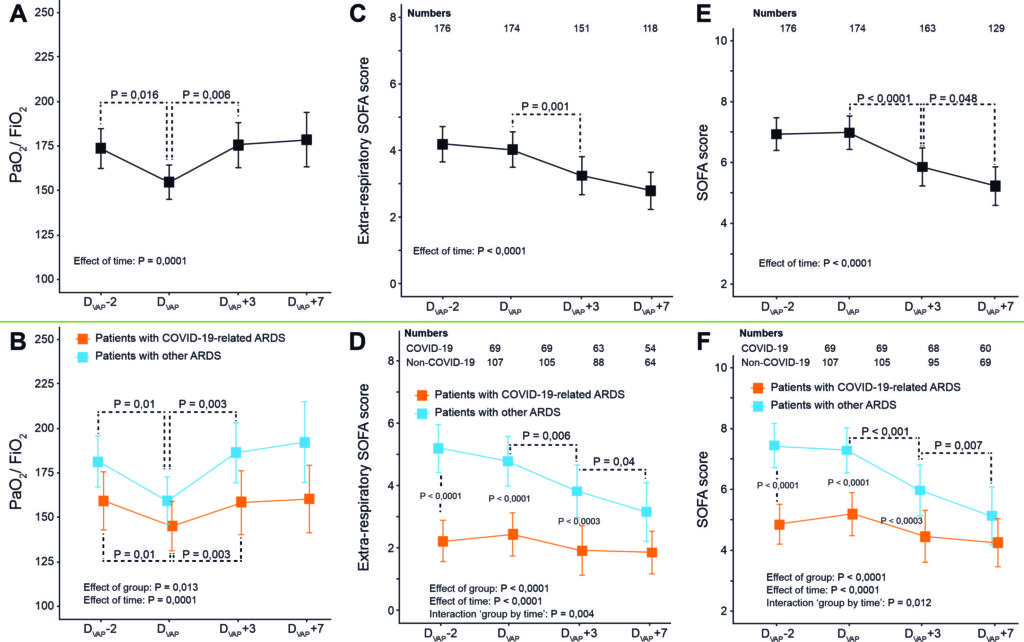
Among the 336 included patients (101 with COVID-19 and 235 with other ARDS), 176 (52.4%) experienced a first VAP. VAP induced a transient and moderate decline in the PaO2/FiO2 ratio without increase in SOFA score values. VAP was associated with less ventilator-free days (median difference and 95% CI, − 19 [− 20; − 13.5] days) and vasopressor-free days (− 5 [− 9; − 2] days) at day 28, and longer ICU (+ 13 [+ 9; + 15] days) and hospital (+ 11.5 [+ 7.5; + 17.5] days) LOS. These effects were observed in both subgroups. Overall day-90 mortality rates were 35.8% and 30.0% in patients with and without VAP, respectively (P = 0.30). In the whole cohort, VAP (adjusted HR 3.16, 95% CI 2.04–4.89, P < 0.0001), the SAPS-2 value at admission, chronic renal disease and an admission for cardiac arrest predicted death at day 90, while the COVID-19 status had no independent impact. When analysed separately, VAP predicted death in non-COVID-19 patients (aHR 3.43, 95% CI 2.11–5.58, P < 0.0001) but not in those with COVID-19 (aHR 1.19, 95% CI 0.32–4.49, P = 0.80).
Conclusions
VAP is an independent predictor of 90-day mortality in ARDS patients. This condition exerts a limited impact on oxygenation but correlates with extended MV duration, vasoactive support, and LOS.
Figure:
Trends in PaO2/FiO2 ratio, extra-respiratory SOFA score values and total SOFA score values in patients with VAP. VAP ventilator-associated pneumonia, ARDS acute respiratory distress syndrome, COVID-19 coronavirus disease 2019, SOFA sepsis-related organ failure assessment. Panels A, C and E, all patients with ARDS; panels B, D and F, patients with COVID-19-related ARDS versus patients with ARDS from other causes