Ref: Nishiura N., et al, J Am Heart Assoc. 2023;12:e025751. DOI: 10.1161/JAHA.122.025751
BACKGROUND: The natural history and optimal interventional timing in patients with isolated severe tricuspid regurgitation (TR) have not been well studied. This study aimed to investigate long-term clinical outcomes and risk factors associated with poor prognosis in patients with isolated severe TR.
Tricuspid regurgitation (TR) is a common echocardiographic finding, and it is encountered in 70% to 90% of the general population. TR has been believed to be a benign disease as it is often asymptomatic and can be managed conservatively with treatments such as diuretic therapy. However, it can sometimes cause right-sided heart failure and require surgical or catheter intervention. Recent studies demonstrated that increased TR severity was associated with higher mortality. Although surgical mortality can be adversely affected by delayed surgical intervention, the optimal timing of intervention for TR remains controversial. A recent study also reported that the prognosis of surgically treated moderate or greater TR did not differ significantly from that treated using medical therapy. Thus, the natural history and risk factors associated with poor outcomes in isolated severe TR remain understudied. Therefore, we aimed to determine the long-term clinical outcomes and risk factors associated with poor prognosis in patients with isolated severe TR to determine the optimal timing for intervention.
METHODS AND RESULTS: Consecutive transthoracic echocardiographic examinations in 2877 patients with isolated severe TR were retrospectively reviewed. Patients with significant left-sided valve disease or repeated examinations were excluded. Primary outcome was defined as a composite of all-cause death and hospitalization for heart failure. Among the 613 enrolled patients (mean age, 74±13 years; men, 38%), 141 died, and 62 were hospitalized for heart failure during the median follow-up period of 26.5 (interquartile range, 6.0–57.9) months. The 5-year event-free rate was 60.1%. TR pressure gradient (adjusted hazard ratio [HR], 1.03 [95% CI, 1.01–1.04]), blood urea nitrogen (adjusted HR, 1.02 [95% CI, 1.01–1.04]), left atrial volume index (adjusted HR, 1.01 [95% CI, 1.002–1.02]), and serum albumin (adjusted HR, 0.56 [95% CI, 0.36–0.95]) were identified as independent predictors of adverse events. A risk model based on the 4 clinical factors that included pulmonary hypertension (TR pressure gradient >40 mm Hg), elevated blood urea nitrogen levels (>25 mg/dL), decreased albumin levels (<3.7 g/dL), and left atrial enlargement (left atrial volume index <34 mL/m2) revealed a graded increase in the risk of adverse events (P<0.001).
CONCLUSIONS: The prognosis of isolated severe TR is not always favorable. Careful attention should be paid to patients with concomitant risk factors, such as pulmonary hypertension, elevated blood urea nitrogen levels, decreased albumin levels, and left atrial enlargement.
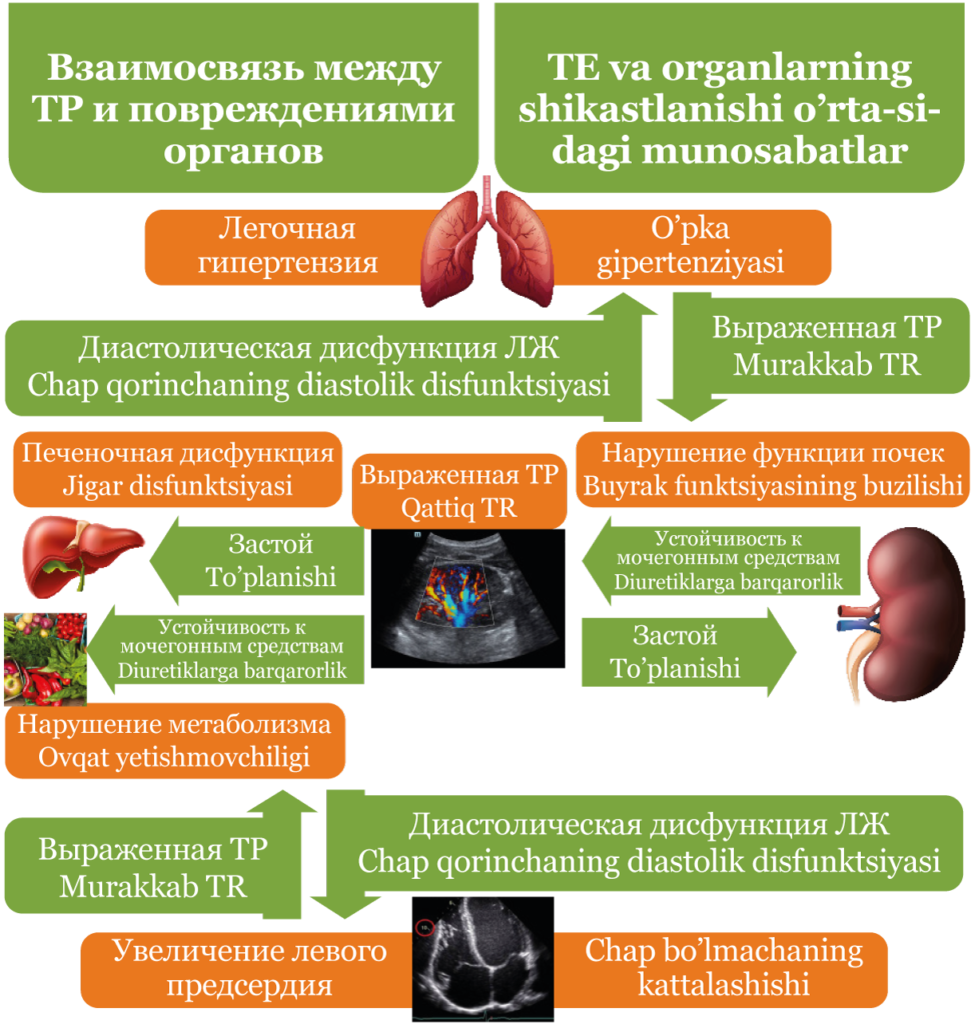
Diagram of association between advanced TR and multiorgan damages. LA indicates left atrial; LV, left ventricular; and TR, tricuspid regurgitation.
CLINICAL PERSPECTIVE
What Is New?
- Patients with severe tricuspid regurgitation may experience adverse events in the long-term.
- A risk model based on pulmonary hypertension, renal and/or liver dysfunction, and left atrial enlargement showed a graded increase in the risk of future adverse events.
What Are the Clinical Implications?
- Intervention might be needed in patients with isolated severe tricuspid regurgitation with concomitant risk factors suspecting multiorgan damages.
- Additional studies are required to evaluate the influence of the interventions on clinical outcomes
in patients with severe tricuspid regurgitation with concomitant risk factors.